
Long considered a disease of older adults, bowel cancer is increasingly affecting younger generations across the globe.
Cases of early-onset bowel cancer are climbing among people under 50 years old, with countries like the United Kingdom, New Zealand and Chile seeing some of the sharpest rises.
Here’s what to know about the shifting landscape of the disease.
What is bowel cancer?
Also known as colorectal cancer, bowel cancer involves tumours in the large bowel, which is made up of the colon and rectum.
Bowel cancer is the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths worldwide, with over 1.9 million new cases and nearly 904,000 deaths reported in 2022.
Where is bowel cancer on the rise?
Bowel cancer is on the rise globally. The World Health Organization projects that by 2040, the annual number of new colorectal cancer cases will rise to 3.2 million.
A new study published in the medical journal The Lancet Oncology found rising bowel cancer rates among younger demographics in 27 of 50 countries studied over a five-year period between 2013 and 2017. Countries with significant annual increases include New Zealand (3.97 percent), Puerto Rico (3.81 percent) and England (3.59 percent).
Advertisement
Historically, the disease has been more prevalent in high-income countries such as the United States, Australia and Canada. However, cases are now also rising in lower-income regions of Latin America and Asia, such as Argentina, Ecuador, Thailand and Turkey.
Countries such as Japan, Chile and Israel, which have undergone rapid urbanization and dietary shifts over the past few decades, are also seeing similar increases in the number of cases among younger people.
What is causing this shift?
The rise in bowel cancer might be related to lifestyle changes in recent years and the resulting modifications to human gut bacteria.
Increased consumption of processed and junk food and sedentary behaviour can be contributing factors to bowel cancer. Generational shifts might also play a role; many individuals in high-income countries born after 1950 were exposed to high-fat, high-sugar and low-fibre diets starting at an early age.
These diets lack protective nutrients like antioxidants and fibre, which help maintain healthy gut cells and eliminate harmful substances such as carcinogens, inflammatory compounds and bile acids produced during the digestion of high-fat foods, which can encourage abnormal cell growth.
Additionally, emerging evidence suggests factors like natural gut microbiome changes and chronic inflammation could contribute to cancer risk, but more research is needed to fully understand their potential impact.
“Gut microbiome” is the community of trillions of bacteria, fungi, viruses and other microorganisms that live in the digestive tract and play a crucial role in digestion, immunity and overall health.
Advertisement
What are the symptoms of bowel cancer?
Symptoms of bowel cancer can vary, but commonly include:
- Rectal bleeding
- Persistent abdominal pain
- Changes in bowel habits, such as diarrhoea or constipation
- Unexplained weight loss
What causes bowel cancer?
Bowel cancer can result from a variety of factors, including lifestyle, genes and the environment.
While family history and inherited genetic mutations increase risk, most cases are sporadic and linked to lifestyle factors. Genetic mutations are naturally occurring changes in the sequence of genes, which provide instructions for how living things grow and function.
Food, alcohol consumption and obesity are other key contributors to the disease. Consumption and high-temperature cooking of red and processed meats can produce carcinogenic compounds, such as heterocyclic amines, increasing the risk of cancerous growths in the colon.
What is the prognosis for bowel cancer?
Treatment depends heavily on the stage of diagnosis.
Early detection typically leads to significantly better outcomes. Around 90 percent of people tend to survive for five years or more if a colon or rectal tumour is detected at Stage 1, before the cancer has spread.
When cancer spreads to other organs, or metastasises, survival rates drop considerably. At Stage 4, the most severe, only around 10 percent of patients survive their cancer for five years or more after diagnosis. However, with cancer, it is not possible to know for sure how long someone will live.
Advertisement
Patients below age 50 often receive more aggressive treatment, such as chemotherapy, alongside surgery, even for early-stage disease. However, studies suggest their survival outcomes are not dramatically better than those of older adults who are less likely to undergo such intensive therapies due to concerns about underlying health conditions or reduced tolerance to side effects.
Who is mostly affected by bowel cancer, and has this changed?
In the past, bowel cancer was more likely to affect people over 50, but the demographic is shifting.
Younger adults aged 25 to 49 are now experiencing the steepest increases in incidence, particularly in high-income countries like the UK, US and Australia.
In countries including England and Norway, women are seeing more increases than men.
Despite this rise, adults over the age of 50 still account for the majority of bowel cancer cases overall.
What are the treatments for bowel cancer?
Treatment for bowel cancer varies by stage and includes several approaches:
- Surgery: Tumours are removed, which is often curative for early-stage cancers
- Chemotherapy: Chemical substances used in combination with surgery aim to prevent disease recurrence
- Radiation therapy: Beams of intense energy are used to kill cancer cells or shrink tumours; this is frequently employed for rectal cancers
- Targeted therapies: Drugs are used to target parts of cancer cells, such as proteins; this can be effective for tumours with specific genetic mutations
- Immunotherapy: Biological therapy boosts a person’s immune system to fight cancer; this is an emerging option, particularly for advanced cases with certain biomarkers
Advertisement
Can bowel cancer be prevented?
Experts suggest that lifestyle changes and regular screenings can significantly reduce risk.
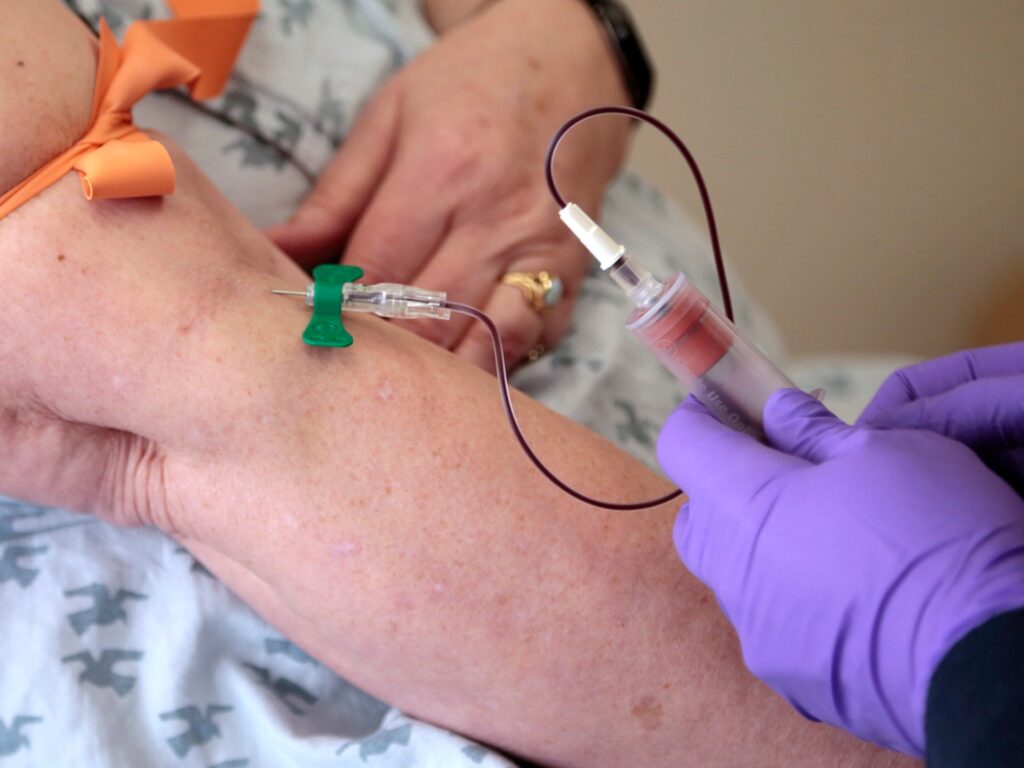
In many countries, including the US and Australia, doctors recommend colonoscopies and stool tests starting at age 45.
Increased awareness of symptoms and family history can also lead to earlier detection and better outcomes.
Studies suggest that maintaining a healthy diet rich in fibre, limiting alcohol consumption, avoiding smoking and staying physically active can also lower risk.










More Stories
African victims of clergy abuse deserve justice and accountability, too
Olmo closer to Barcelona exit after registration request rejected
Turkiye to allow pro-Kurdish party to visit jailed PKK founder